Prostate-specific membrane antigen (PSMA) theranostics has shown promising results in both diagnosis and treatment of prostate cancer and is becoming an increasingly important tool in the management of this disease.
Several studies have demonstrated the effectiveness of PSMA PET imaging in detecting and localizing prostate cancer with high sensitivity and specificity, and PSMA-targeted radionuclide therapy has shown promising results in improving survival and quality of life for patients with advanced prostate cancer.
Despite its name, PSMA is not prostate-specific. PSMA expression is also found in a multitude of non-prostatic diseases including a subgroup of sarcomas, mostly in its neovascular endothelial cells. On PET/CT imaging, multiple sarcomas have also shown intense PSMA-tracer accumulation. PSMA expression and PSMA-tracer uptake seem to be highest in patients with aggressive and advanced sarcomas who are also in highest need of new therapeutic options.
Several studies have explored the potential use of PSMA-targeted imaging and therapy in osteosarcoma. One study found that PSMA expression was detected in 46% of osteosarcoma samples, while no PSMA staining was observed in osteofibrous dysplasia. More importantly, the expression of PSMA is correlated with tumor size, pulmonary metastasis and worse survival, with a survival rate of 63.2% in the PSMA-negative group versus 36.6% in the PSMA-positive group [1].
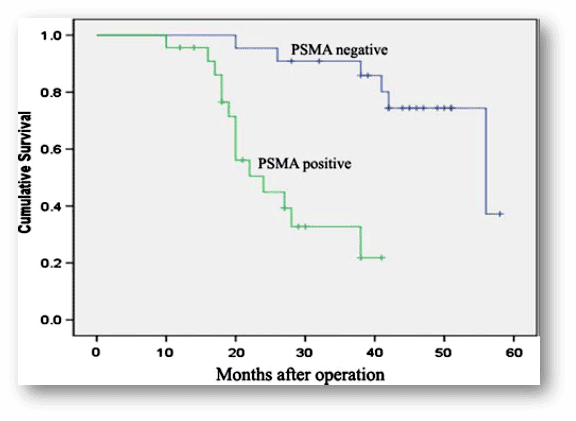
PSMA expression was associated with worse survival in osteosarcoma patients by Kaplan–Meier analysis [1]
The following images published by Arun Sasikumar et al. [2] show how 68Ga-PSMA PET/CT can differentiate Osteosarcoma from Fibrous Dysplasia (FD).
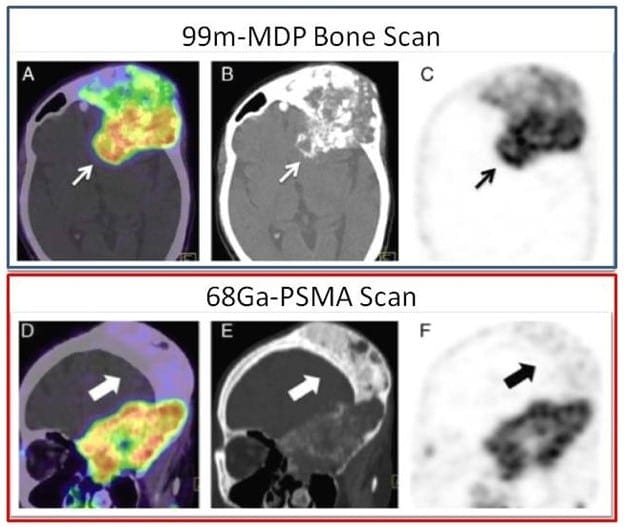
68Ga-PSMA PET/CT showed selective tracer uptake in the areas of sarcomatous changes (A, fused PET/CT image; B, CT image; C, PET images, small arrows) with characteristic CT changes. Only minimally increased tracer uptake is noted in the regions of FD (D, fused PET/CT image; E, CT image; F, PET images, large arrow). The selectively increased tracer uptake is also appreciable in the maximum intensity projection images.
Malignant transformation in FD is rare, and osteosarcoma, fibrosarcoma, and chondrosarcoma are the common malignancies developing in FD.
Neither Tc-MDP bone scan nor F-FDG PET/CT can differentiate between FD and areas of malignant transformation in FD.
An immunohistochemistry-based study showed positive staining for PSMA in osteosarcoma and no PSMA staining in FD.
In the above case [2], intense tracer uptake was noted in areas of sarcomatous change, with no abnormal uptake in areas of FD with no malignant transformation.
This case highlights the ability of 68Ga-PSMA PET/CT to map tumor neoangiogenesis in osteosarcoma arising in FD, which can have potential theranostics implications.
While these results suggest that PSMA-targeted approaches may have potential for the management of osteosarcoma, further research is needed to evaluate their efficacy and safety in human patients [3].
References:
- Zeng C., Ke ZF., Yang Z. et al. Prostate-specific membrane antigen: a new potential prognostic marker of osteosarcoma. Med Oncol29, 2234–2239 (2012).
- Arun Sasikumar, Ajith Joy et al. 68Ga-PSMA PET/CT in Osteosarcoma in Fibrous Dysplasia. Clin Nucl Med 2017;42: 446–447.
- Kleiburg F., Heijmen L., Gelderblom A.J. et al. Prostate-specific membrane antigen (PSMA) as a potential target for molecular imaging and treatment in bone and soft tissue sarcomas. The British Journal of Radiology. 2/2/2023 DOI: 1259/bjr.20220886

Haim Golan
MD MSc
Chief Medical Officer
Isotopia Molecular Imaging LTD